Are you interested in providing feedback on this webpage? Please fill out our evaluation here.
- Non-modifiable risk factors, including family health history, when we got our first period, what age we had babies or if we gave birth at all, are the risk factors that we are unable to change. However, there are steps that we can take early on to understand how they play a role in our overall risk.
Genetics & Family History
Breast Density
Age

Hormones and Menstrual History
- You have a higher risk of developing breast cancer if you have a strong family history of breast cancer on your mother or father’s side, or have certain gene mutations.
You are at 2x higher risk of developing breast cancer if a first-degree relative (mother, sister, daughter) has had breast cancer. This risk further increases if you have more than one affected first degree relative or if they received the diagnosis before menopause. - It is also important to know if second-degree relatives (aunts, nieces, granddaughters) have had a breast or ovarian cancer diagnosis, especially at a young age.
- Certain genes in the body, called BRCA 1 AND BRCA 2, are responsible for protecting you from developing breast and ovarian cancer. There are 18 other genes that also function the same way.
- A mutation occurs when there is a change to one of these genes. A BRCA-1 or BRCA-2 mutation can increase your lifetime risk of developing breast cancer. BRCA-1 and BRCA-2 genes can be inherited from either your mother or father.
- Testing for these gene mutations is done by a blood test or spit test.
Why is this important to Black women?
- Some research from around the globe shows us that Black women, or women of African or Caribbean ancestry, may have a higher prevalence of BRCA1/2 mutations and may not know it. 1-4
- There are other mutations associated with breast cancer (PALB2 and TP53) that Black women may be at an increased risk of having. 5, 6
- In the United States , Black women often face challenges to getting genetic testing, including language barriers and costs. Health care providers are also less likely to discuss genetic testing with Black women than White women in the U.S. 7 Genetic testing is covered for high-risk individuals in Canada, however it is still important to be aware of the importance of your family history and the option for genetic testing.
What does this mean for me?
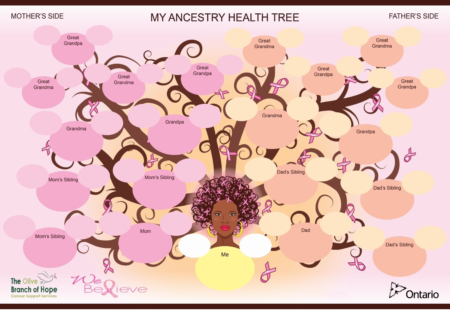
- An important first step is identifying your family history of breast and ovarian cancer . This can be challenging if family members don’t know their history, don’t want to share, or if you don’t feel comfortable asking.
- Finding this information may help you decide when you should start screening for breast cancer with a mammogram, with other breast imaging tools, or if you should have genetic testing done.
- Some women with a significant family history might be advised to start annual mammograms at age 40, or 10 years before the cancer was diagnosed in the close family relation.
- If you do find a family history of breast or ovarian cancer, starting a conversation with your healthcare provider about your history is a good first step.
The Olive Branch of Hope’s Family Tree Guide
How can I access genetic testing?
Genetic Counsellors assess your personal and family medical history to see if you may have a high risk of developing cancer. A Genetic Counsellor can also discuss if genetic testing is appropriate for you.
In Ontario, Ontario Health Insurance Plan (OHIP) coverage for genetic testing is limited to those who meet certain criteria. Some of these criteria include a positive family history of cancer and young age at diagnosis. For more information on eligibility, see Cancer Care Ontario’s Guidelines and Advice for Screening for Women at High Risk here. For women outside of Ontario, check your jurisdictional guidelines and recommendations.
Without meeting these criteria, genetic testing can cost between $900-$1500. However, If you do not meet the criteria for OHIP-covered genetic testing but are interested to know if you are at a high risk of breast cancer due to a BRCA mutation, you can enroll in The Screen Project. The Screen Project is a national initiative that aims to make BRCA screening available to all Canadians over 18+, at a reduced cost of $250 U.S.
Note:
It is also important to note that most women develop breast cancer without having a family history, as genetic factors only account for 5-10% of all breast cancer cases.
What is breast density?
- Breasts are made up of 3 types of tissues: fatty, glandular, and fibrous (connective) tissue. The more glandular and fibrous tissue your breasts have, the denser they are.
- Breast density can be inherited, and the amount of dense tissue in your breast varies between women. Having more density is more common among younger women.
How dense are my breasts?
- The amount of breast density can be determined by images from a mammogram. A mammogram is an x-ray examination of the breast used to screen for signs of breast cancer. Here are 5 things you need to know about mammograms.
Using a system called BI-RADS, the density in your breast is classified into four groups, from A to D.
BI-RADS A: there are mainly fatty tissues in the breast
BI-RADS B: there are few regions of dense (glandular and fibrous) tissues
BI-RADS C: there are approximately equal parts of fatty and dense tissue in the breast
BI-RADS D: almost all of the breast is dense tissue (extremely dense)
Having dense breasts (type C or D) does not mean that you will develop breast cancer, but it increases your risk. This is because many breast cancers are formed in the glandular and fibrous tissues, which dense breasts have more of. It can also be more challenging to find breast cancer in dense breasts.
Why is this important to Black women?
- Some U.S. research shows that Black women may be more likely than White women to have dense breasts, putting them at greater risk of developing breast cancer.8 However, other research claims this is not the case.9
- Although the findings are unclear, it is important to understand how breast density might be a risk factor for breast cancer and to become breast aware.
What does this mean for me?
- It is important to be breast aware because you are the expert on your body. Keep a close eye on how your breasts usually look and feel. If you notice any changes, talk to your healthcare provider.
If you do get a mammogram, have a conversation with your health care provider about breast density and your breast density score.
Mammograms alone may not be enough for women with dense breasts because it is more challenging for radiologists to detect the presence of cancer if the breast tissue is extremely dense. However, if you have extremely dense breasts, it is still important to get mammograms regularly. Sometimes other tests (ultrasound and on rare occasion MRI) are suggested for a more accurate examination of your breast tissue.
Age is a significant risk factor for developing breast cancer. Our cells are always dividing and making new copies of themselves. As we age, there are more opportunities for mistakes to happen when the cells divide, and sometimes cells can overgrow and clump together to form tumors. In general, most breast cancer cases are found in women over the age of 50, with 62 years being the average age of breast cancer diagnosis.
Why is this important to Black women?
- In the United States, most women who get breast cancer under the age of 45 are Black.10
- In the United States, younger Black women have a high risk of developing triple-negative breast cancer– a more aggressive form of cancer.11
- Black women may be at risk of breast cancer developing at younger ages than the average population, and in this younger age group the breast cancer that is diagnosed may be more aggressive.
What does this mean for me?
- It is important to speak to your health care provider to discuss your personal risk of breast cancer and think about when breast cancer screening should start for you.
This may mean a mammogram that may take place earlier than what is recommended for the average population. - Routine screening for women at average risk for breast cancer starts at age 50 based on the guidelines of the Canadian Task Force on Preventive Health Care. As many women do not know whether they are at average or higher than average risk, the Canadian Cancer Society and many physician led organizations recommend that women age 40 to 49 , talk with their healthcare provider about the limitations and benefits of having a mammogram.
- It is important to be breast aware at any age, as you are the expert on your body. Keep a close eye on how your breasts usually look and feel, and if you identify any changes, talk to your healthcare provider.
- Persistent changes in one breast should be investigated with an ultrasound if you are less than 30 or are pregnant or breastfeeding, and a mammogram and ultrasound if you are 30 or older.
There are specific hormonal factors associated with a higher risk of breast cancer, such as:
- Getting your period before age 12
- Reaching menopause after age 55
- Having your first baby after age 30
- Never having a full-term pregnancy at all
Why is this important to Black women?
- We still have more to learn about how hormones and menstrual history present as risk factors for Black women. There will be more information as more research is done.
What does this mean for me?
- Many women can identify at least one of these risk factors in their health history, but most will not go on to develop breast cancer. The most important thing is to talk to your health care provider about what these risk factors mean for your personal health and your risk of breast cancer.
- Breast feeding can reduce a woman’s risk of developing breast cancer, specifically aggressive forms such as triple-negative breast cancer. Breastfeeding delays a woman’s menstrual cycle, reducing exposure to hormones such as estrogen which are known to increase the risk of breast cancer.
- However, we recognize that breastfeeding can be challenging for new mothers. If you are having difficulties with breastfeeding, talk to your provider about connecting you with a lactation consultant.

References | Glossary | Graphics Designed Nafisa Salima
This site is best viewed on Chrome








