By Jordan Benadiba

As an embedded researcher, Rachael Bosma has a front row seat to the routine clinical challenges that come with caring for patients living with chronic pain. “As the research lead for the Toronto Academic Pain Medicine Institute (TAPMI), I leverage research insights to both address these issues and study the impact they have on patient care,” Bosma shared.
A key challenge facing chronic pain medicine is wait times. “In our experience, patients who have had to wait a long time to see specialty care often come in for their first appointment expecting answers and relief for their pain. They often assume that they will receive a diagnosis and treatment or medication that day that will address their issue,” Bosma said. “Unfortunately, chronic pain is a chronic disease and there is no panacea. Patients need to engage in ongoing self-management behaviours to improve their health, and this can be difficult to hear especially if this is the first time they are being told that they have a chronic disease.”
Given this reality, Bosma and colleagues created a web-based interactive self-management program to support patients before their first appointment TAPMI’s pelvic pain clinic. The goal was to provide self-management education to patients now rather than waiting until their first visit. When the patient does come into the clinic, their care team can build on what they have already learnt and started to implement through the self-management program.
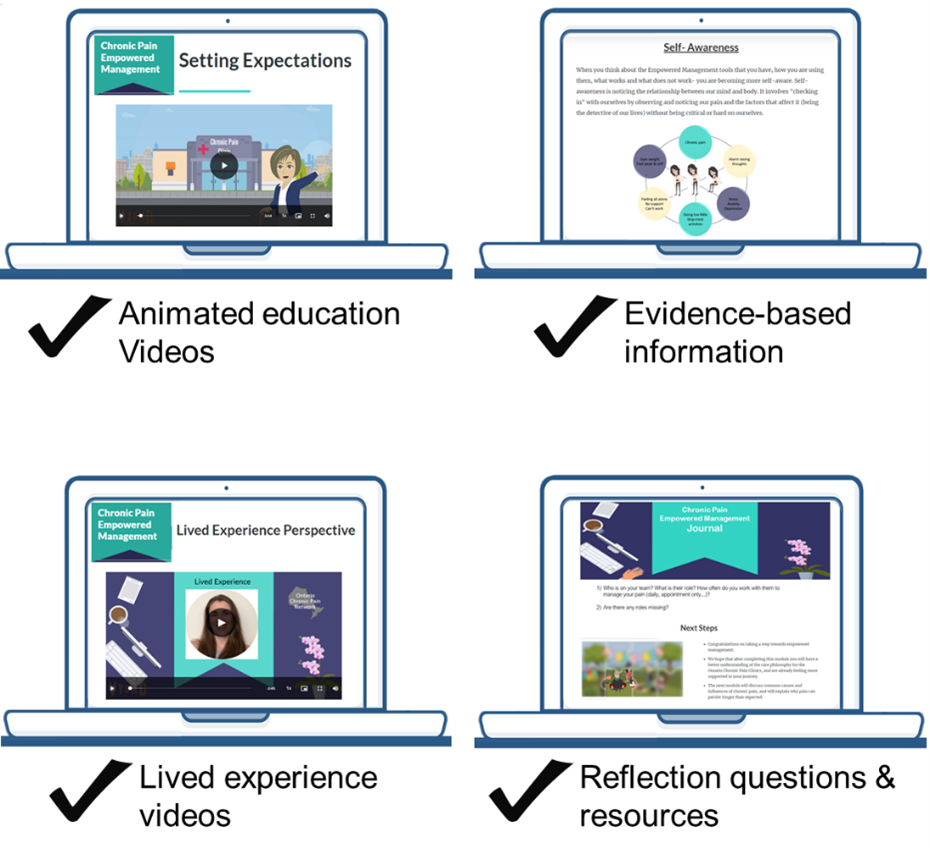
After evaluating its feasibility and acceptability, Bosma and team built on this concept to create an empowered management program for chronic pain more generally. Developed in collaboration with researchers at Queen’s University and other sites, the motivational empowerment program includes a series of eight interactive web-based educational modules. To ensure its effectiveness and real-world applicability, the program was co-designed with chronic pain patients, who provided insights regarding program content, design, and usability. The empowered management program also includes a reflection journal and can be enhanced through one-on-one coaching sessions.
“Wait times for chronic pain care are not unique to Toronto or even Ontario,” Bosma stated. “Providers across the country need more supports for their patients experiencing chronic pain. As a result, we believed that the empowerment management program needed to have a national platform.”
By the end of this year, the program will launch on the Power Over Pain portal, a new virtual platform co-created by a diverse group of researchers, clinicians, and Canadians with chronic pain. The Power Over Pain platform includes self-assessment tools with bi-weekly check-ins to help guide decision-making on interventions and provide users with feedback on their mood, anxiety, pain, and sleep. The platform also leverages evidence-based virtual pain interventions, like TAPMI’s empowered management program, that are delivered in a stepped care manner based on the individual’s needs.
“Power Over Pain is for anyone in Canada living with chronic pain. Our hope is that community care providers, like family physicians, refer their patients to the platform and utilize the tools available,” Bosma explained. “In some cases, and depending on the individual’s unique needs, they may not need a referral to a specialty chronic pain clinic after utilizing Power Over Pain.”
To address pervasive and chronic health system challenges, like wait lists, innovative and evidence-based solutions need to be spread and scaled across the country. In the field of chronic pain, TAPMI is leading the way.