Genetic testing is a powerful tool used to detect changes in our genes that can be associated with a greater risk of developing certain cancers, including breast cancer. While genetic testing rates are on the rise, Black women’s participation remains low. Reasons for low participation include lack of knowledge and awareness about genetic counselling and testing, cost of testing, distrust of the healthcare system, ineffective communication from healthcare providers, lack of referrals from healthcare providers, and various family concerns.
Take Action, Take Control is a new initiative to empower Black women to take action and take control by learning more about what hereditary cancer genetic testing can mean for them and their families. Through this initiative, The Peter Gilgan Centre for Women’s Cancers at Women’s College Hospital will provide information about hereditary cancer genetic testing tailored to Black women to allow them to feel heard, seen and represented.
Are you finding the information presented in this webhub helpful?
We value your feedback. Please consider completing this two-minute anonymous questionnaire to help us understand if you found this webpage useful and how we can make it even better.

Risks And Benefits of Hereditary Cancer Genetic Testing
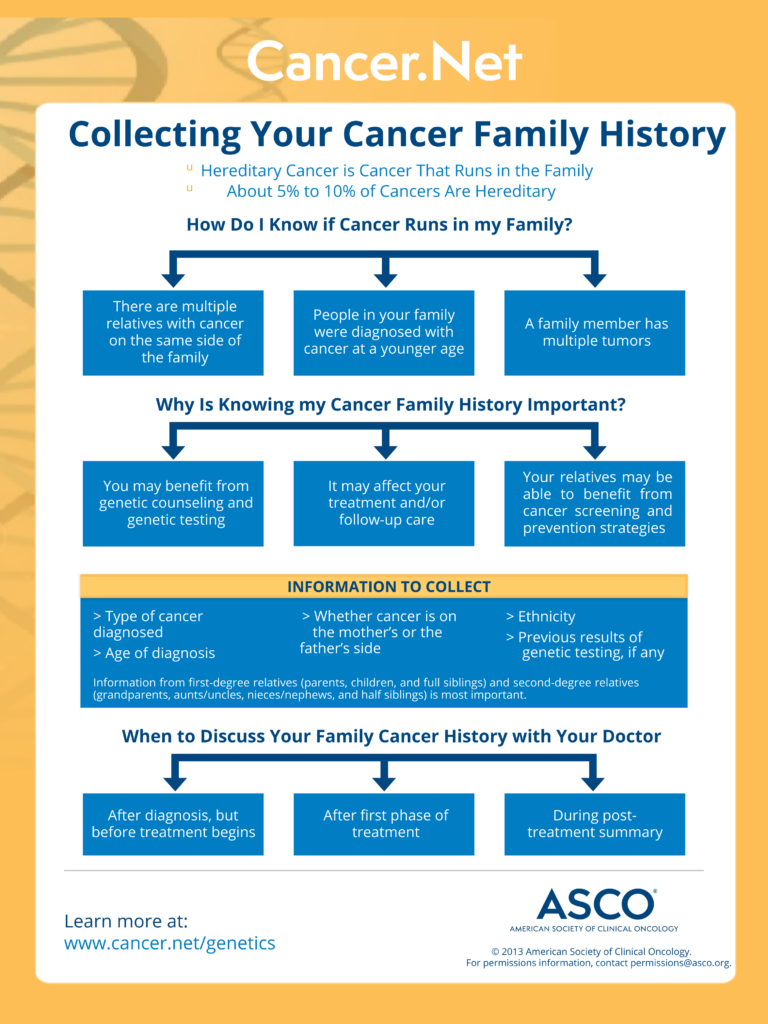
Choosing to have genetic testing is a personal decision. Some people are encouraged to consider testing if they have a personal or family history of certain cancers. When thinking about your family history of cancer, consider both sides of your family. Hereditary cancer can come from either your mother or your father. Discuss your personal and family history of cancer with your primary care provider to help you decide if testing is right for you.
For some people, genetic testing may provide answers to questions about their family history or personal history of cancer. It may also relieve anxiety or uncertainty about their cancer risk. If you are found to have a mutation that increases your risk of cancer, knowing this may help you to take steps to reduce your risk of cancer. It could also help you make decisions about treatment if a cancer develops. Genetic testing results may also help your family members to make decisions about their health.
Genetic mutations that can increase a person’s cancer risk can be related to multiple cancers. For example, mutations in the BRCA1 and BRCA2 genes are associated with breast, ovarian, and prostate cancers. Mutations in other genes may be associated with other cancers such as colorectal and pancreatic cancers. Therefore, it is important to think about your personal and family history of all types of cancers, not just breast cancer.
Most people who seek genetic testing based on their personal and/or family history of cancer will not have a mutation identified in them. However, if a mutation is found, some people may feel distressed or anxious after learning that they have a higher risk of cancer. Some people also find it difficult to share or discuss their testing results with family members. Some may have feelings of guilt that they may have passed down a gene mutation to their child. If you are unsure, discuss your concerns with a genetic counsellor or your primary care provider. They can help you decide whether testing is the right decision for you at this time. If you decide to have genetic testing, they can also provide you with tools and advice for dealing with the challenges that may follow after getting your results.
What To Expect If You Seek Genetic Testing
In the past, breast cancer patients in Ontario were tested for mutations in just two genes (BRCA1 and BRCA2). However, scientists have since discovered many more genes that, if mutated, may increase a person’s risk of developing cancer. As a result, tests have expanded, and patients can choose large multi-gene panels (typically 19 genes or more). Speak to your genetic counsellor to understand which genes will be tested if you decide to seek testing.
Genetic testing requires a sample of your DNA. Typically, a DNA sample is taken from saliva, a cheek swab, or a blood sample. The type of sample needed will be determined by the clinic and/or lab that provides your test. Ask your genetic counsellor about what type of sample would be required if you decide to have genetic testing.
The time it takes to get your results after you provide your DNA sample will depend on the lab that does your test. For most people, it usually takes 2 to 8 weeks to receive the results of their genetic test. Typically, your genetic counsellor will contact you to review your results, discuss what they could mean for you and your family, and plan for next steps, if applicable.
There are three possible results of a genetic test:
1) POSITIVE: a mutation was detected
2) NEGATIVE: no mutations were detected
3) UNCERTAIN: a genetic variant of ‘uncertain significance’ was identified.
- POSITIVE. This means that you may have an increased risk of developing certain types of cancer. As a result, your genetic counsellor or doctors may recommend:
- increased screening for certain cancers;
- changes to your treatment if you have already been diagnosed with cancer;
- steps to reduce your risk of or prevent certain cancers;
- that your family members consider genetic testing.
- NEGATIVE. This means that the chance that you have a hereditary risk for cancer is much lower. You should still talk to your healthcare provider about cancer screening and risk reduction based on your personal risk factors and/or family history of cancer.
- UNCERTAIN. This means that there was a genetic change or difference identified in your DNA. However, it is not yet known if that specific genetic change increases your cancer risk or not. Remember, we all have genetic differences which make us unique. Most of these genetic differences are completely harmless and do not increase our risk for cancer or any other condition. Your genetic counsellor can provide additional information about variants of uncertain significance and what it may mean for you and your family members. Typically, an uncertain result will not change your recommendations for cancer screening or treatment.
Accessing Genetics Services
Talk to your primary care provider to find out if you are eligible for a genetics assessment. If your primary care provider recommends an assessment, they will refer you to a genetics clinic in your area. The Canadian Association of Genetic Counsellors provides a directory of genetics clinics on their website. If you are in Ontario, Ontario Health also provides a directory of genetics clinics on their website.
If you are not eligible for a genetics assessment or the cost of testing will not be covered by your provincial healthcare system, there are other options.
Some initiatives, like The Screen Project, may provide access to reliable pay-for-service genetic testing. To find out more, visit their website.
Some independent laboratories or companies also offer pay-for-service hereditary cancer genetic testing. This means you can buy genetic testing kits or services from private companies. However, not all laboratories/companies provide clinical-grade testing and counselling services. Ask your primary care provider or genetic counsellor about trustworthy and reliable options.
After you get a referral to a local genetics clinic, you will likely meet with a genetic counsellor. The genetic counsellor will estimate your risk for hereditary cancer based on your personal and family history. They will also check if you meet provincial eligibility criteria for testing. If you meet the criteria, the genetic counsellor will discuss:
- the risks and benefits of testing, and
- how this information can impact you and your family.
The Ontario Health Insurance Plan (OHIP) pays for genetic testing for those who meet specific eligibility criteria. To check if you are eligible, a genetic counsellor will review your personal and family history of cancer. Eligibility criteria may be different in each province/territory.
If you do not meet the criteria for your province/territory, there are other options for testing. However, these other options typically come at a cost. See ‘How do I access genetics services?’ for more information.
The DNA that we were born with does not change over time. If a person does a genetic test today and does the exact same test again in the future, the results will not change. However, in the future we may discover additional genes that we can analyze, and our testing technology may get even better at detecting mutations present in the genes that are analyzed. Keep in touch with your genetic counsellor and/or healthcare provider to learn if/when new testing becomes available.
In the past, breast cancer patients in Ontario were tested for mutations in just two genes (BRCA1 and BRCA2). However, scientists now know about other genes that, when mutated, can increase a person’s chance of developing breast, ovarian, and other cancers. Therefore, the testing now available is much more extensive. Patients are now being offered tests that look at 19 genes or more and the turnaround time to get results is also much faster. Speak to your healthcare provider or genetic counsellor to discuss whether doing another test that looks at more genes would be useful for you and your family members.
There have been changes to the eligibility criteria for hereditary cancer genetic testing in Ontario. Many more patients can now have their genetic testing paid for by the Ontario Health Insurance Plan (OHIP). Check with your healthcare provider or genetic counsellor to see if you meet the new criteria.
Are you finding the information presented in this webhub helpful?
We value your feedback. Please consider completing this two-minute anonymous questionnaire to help us understand if you found this webpage useful and how we can make it even better.

- The website of the Canadian Association of Genetic Counsellors provides information about genetic counsellors and genetic testing. Under the “Ask a GC” page, you can submit a question to be answered by a volunteer genetic counsellor.
Are you finding the information presented in this webhub helpful?
We value your feedback. Please consider completing this two-minute anonymous questionnaire to help us understand if you found this webpage useful and how we can make it even better.

 | Elysia Bryan Breast Cancer Survivor & BRCA2 Mutation Carrier |
 | Michelle Audoin Michelle Audoin is a creator, community collaborator, and changemaker living with metastatic breast cancer who advocates for equity, diversity, and inclusion in cancer care. She partners with organizations, like Women’s College Hospital, by drawing on her living experience to work towards supporting systemic change. Connect with Michelle via Instagram @michelle_audoin |
 | Canadian Cancer Society The Canadian Cancer Society (CCS) is a national, non-profit, community-based organization that is dedicated to eradicating cancer and improving the quality of life of people living with cancer. |
 | TAIBU Community Health Centre TAIBU Community Health Centre offers Black-identifying clients from throughout the Greater Toronto Area access to primary care, health promotion and disease prevention programs in a culturally affirming environment. |
 | Rethink Breast Cancer Rethink Breast Cancer is a Canadian charity known for making positive change and rethinking the status quo when it comes to breast cancer. Rethink educates, empowers and advocates for system changes to improve the experience and outcomes of those with breast cancer. |

- Elaine Goulbourne – Director, Peter Gilgan Centre for Women’s Cancers, Women’s College Hospital
- Dr. Aisha Lofters – Chair in Implementation Science, Peter Gilgan Centre for Women’s Cancers, Women’s College Hospital
- Camille Williams – Innovation, Spread and Scale Lead, Peter Gilgan Centre of Women’s Cancers, Womens College Hospital
- Angelina Tryon – Genetic Counsellor, Women’s College Hospital
- Dr. Mohammed Akbari – Scientist, Women’s College Research Institute
- Emma Rinaldo – Social Worker, Women’s College Hospital
- Maria Madden – Communications Advisor, Strategic Communications, Women’s College Hospital
- Ariana Del Bianco – Canadian Cancer Society
- Tameika Shaw – TAIBU Community Health Centre
- MJ DeCoteau – Rethink Breast Cancer