Rationale and Background
Public Health authorities have begun a national roll-out of two COVID-19 vaccinations (Pfizer-BioNTech COVID-19; Moderna COVID-19) to prioritized populations, including segments of First Nations, Inuit, and Métis communities. Despite the prioritization of these populations, there may be barriers to the uptake of COVID -19 vaccinations across our communities for numerous complex and context-specific reasons. One of the barriers identified by our communities and by service providers, decision-makers, Elders and Knowledge Keepers is a lack of culturally safe and relevant educational materials about vaccination. It is critical to address this need urgently due to the rising rates of covid within some of our communities as well as the ongoing barriers related to a lack of cultural safety in the healthcare system.
FIRESIDE CHATS
Confirmed First Nations, Inuit and Métis Healthcare Professionals, Traditional Practitioners & Trusted Community Members:
COVID-19 VARIANTS
Indigenous Languages Translations: Interactive PDF Guides
- Eastern Ojibwe
- Ojibwe-Cree
- Cree
- Mohawk
- Cree
- Michif
- Waneek Horn-Miller, Mohawk Olympian, Mother & Motivator
- Dr. Ojistoh Horn, Bear Clan Family physician from Kahnawake, Working in Akwesasne
- Kahentinetha Horn, Otiskareh:Wakeh — Spitting Bear Clan, Kahnawake
- Leonard Benoit, Qualpi Mi’kmaq Indigenous Patient Navigator—Wolf Clan Organization: Toronto Regional Cancer Program
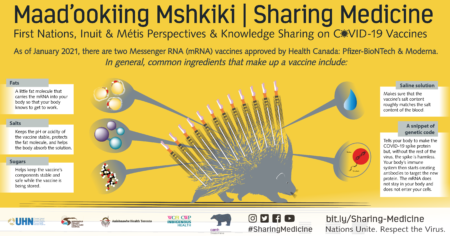
What’s in the Messenger RNA (mRNA) vaccines approved by Health Canada: Pfizer-BioNTech & Moderna & how do they work? – download .pdf
COVID-19 Vaccines – download.pdf
- Dr. James Makokis, MD., M.H.Sc, CCFP
Organization: CAMH; University of Toronto; University of Alberta
Affliations: Medical Director, Shkaabe Makwa, CAMH; Associate Clinical Professor, Department of Family Medicine, University of Alberta; Adjunct Faculty, Dalla Lana School of Public Health, University of Toronto - Dr. Lisa Richardson, MD, MA, FROC Strategic Lead in Indigenous Health
Organization: Women’s College Hospital, University Health Network, Temerty Faculty of Education, University of Toronto
Affiliations: Staff physician, General Internal Medicine, University Health Network; Strategic Lead, Indigenous Health, Women’s College Hospital & Faculty of Medicine, University of Toronto; Co-Chair, Indigenous Health Program, University Health Network - Cheryllee Bourgeois, Exemption Métis Midwife
Organization: Seventh Generation Midwives Toronto; Call Auntie Clinic
Affiliations: Assistant Professor, Ryerson University, Midwifery Education Program
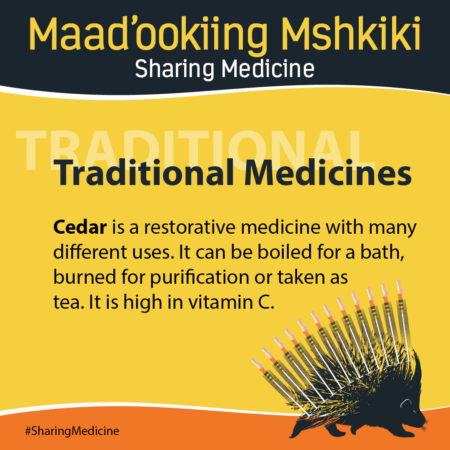
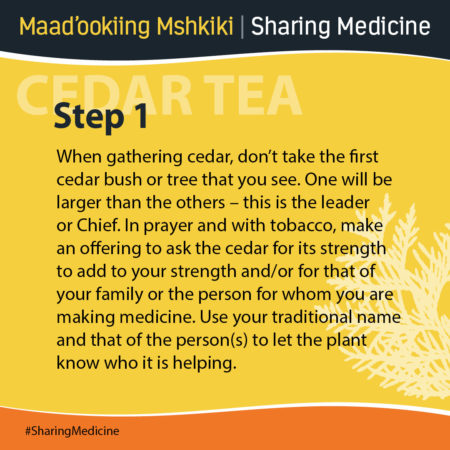
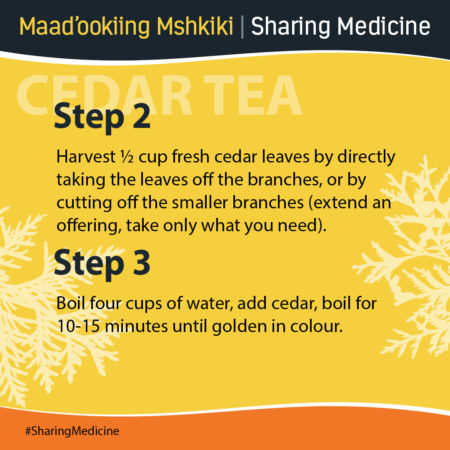
Intersections Between Biomedicine & Traditional Knowledge(s) & Medicine(s)
- Dr. Karen Hill, MD.D, CCFP, Assistant Professor
Organization: Department of Family Medicine McMaster University
Affiliations: Co-Auntie “The Aunties Dandelion” Indigenous community-based engagement, films, lectures, workshops and research support. - Dr. Amy Montour, BScN, MSc, MD, CCFP (PC)
Organization: McMaster University
Affiliations: Brant Community Health Care System
Haudenosaunee, Six Nations of the Grand River Territory - Elva Jamieson, Traditional Medicine Practitioner /Teacher – Lead
Organization: Juddah’s Place
Affiliations: Six Nations Family Health team, Soahac =Chippewa, London, Windsor, Owen Sound,
Oneida Medical Centre, Ogwanohgwatrae:’ Six Nations Traditional Medicine, Aamjiwnaang Health Centre, Sarnia,K/Gaweniyo Schools, Cultural Immersion School
Six Nations, Cayuga Nation, wolf clan of the Six Nations confederacy located at Six Nations of the Grand River Territory. - Ashley Montour, BSc, RPN
Haudenosaunee, Six Nations of the Grand River Territory
- Clay Shirt, Knowledge Keeper
Organization: Waakebiness-Bryce, Dalla Lana School of Public Health at the University of Toronto
Wolf Clan of Saddle Lake Alberta, Treaty 6 - Pauline Shirt, Cree Spritual Consultant
Affiliations: Co-founder of the Kapapamahchakwew – Wandering Spirit School
Red-Tail Hawk Clan of Saddle Lake Alberta, Treaty 6 - Luanna Shirt, Indigenous Cultural Knowledge Educator/ Indigenous Language Advocate
Nehiyaw/Anishinaabe Kwe/Bizhiw Dodem - Les Harper
- Dee Sheridan
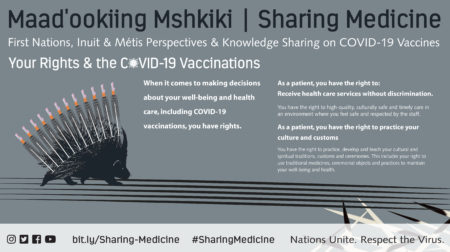
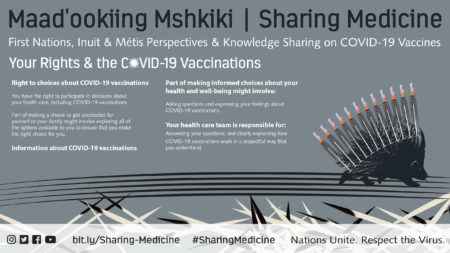
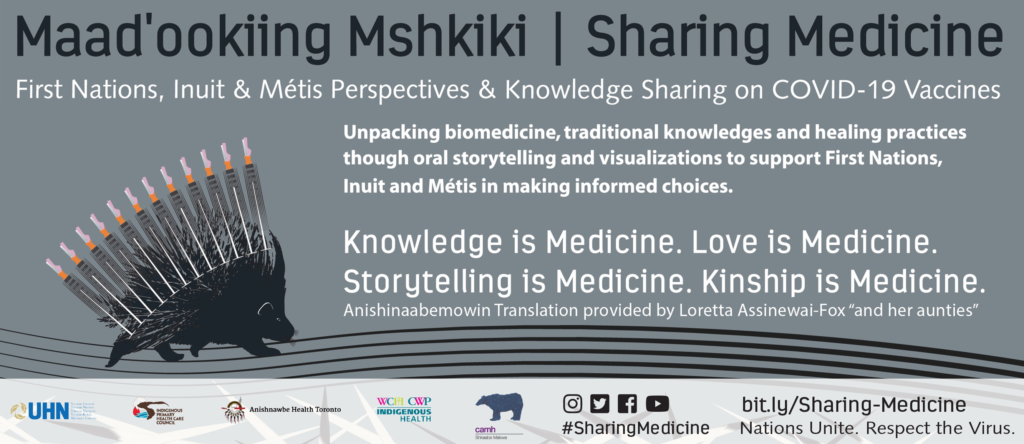
This project aims to build on other community-led and allied initiatives that share the goal of advancing access to quality and safe healthcare services for our communities and meeting the needs of those who are systemically marginalized. Specifically, this project aims to provide timely, accurate, trauma-informed, and culturally relevant information about medical concepts related to available COVID-19 vaccinations with the explicit aim of empowering informed consent and decision making of First Nations, Inuit and Métis peoples living in urban and related homelands.
The Centre for Wise Practices in Indigenous Health (CWP-IH) in partnership with Indigenous Primary Health Care Council (IPHCC), Anishnawbe Health Toronto (AHT) and The University Health Network, Indigenous Health (UHN) and Shkaabe Makwa (CAMH) will develop public-facing and community-centered informational resources/ tools (i.e., video blogs and infographics) tailored for First Nations, Inuit and Métis communities. Using a strength-based, relatable approach that resonates, this initiative will provide accessible resources that recognize and respect Indigenous worldview(s), rooted in upholding principles and standards of Indigenous knowledge translation through oral storytelling; sharing traditional knowledge(s) and healing practices that can build immunity with western biomedical scientific information and acknowledging traumatic experiences in healthcare.
- Design information products and tools that use plain language while ensuring that materials are culturally and contextually relevant for First Nations, Inuit and Métis peoples living in urban and related homelands
- Highlight additional resources related to available COVID-19 vaccinations, beyond the scope of this initiative, aligned with the key project objectives and overarching commitments
- Adopt a variety of methods to deliver messaging (e.g., social media, websites, radio, print, videos) to ensure communication is accessible and reaches as many people as possible
- Draw on personal experiential narratives from First Nations, Inuit and Métis storytelling practices to explain statistical, western biomedical and public health information specific to COVID-19 transmission, spread and prevention
- Bring facts to life and model behaviour(s)/values of:
- kind honesty, integrity, humility, wisdom, love, respect, relevance, responsibility, reciprocity, courage, bravery
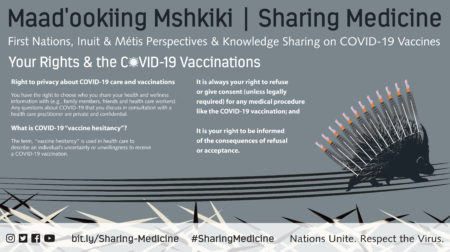
- Use decolonial approach and framework to situate and unpack the concept of “vaccine hesitancy”, address the relationship between biomedicine and traditional knowledge and medicine, and explain COVID-19 vaccinations
FOCUS OF MESSAGING: CIRCULATING AROUND MENTAL, EMOTIONAL, SPIRITUAL & PHYSICAL WELLBEING
All Research: harnessing community and peer-reviewed evidence (updated daily) and regulatory recommendations from the Centre for Effective Practice.
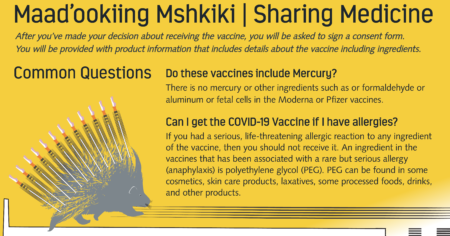
- Ingredients and allergies.
- Possible side effects.
- Where to get vaccinations.
- Differences between vaccines.
- How are they administered.
- Who are they currently available for.
- Complimentary practices.
- The relationship between biomedical definitions of health and culturally situated definitions of wellbeing.
- Drawing from both systems of knowledge.
- How might it be related to colonial histories and ongoing experiences of anti-Indigenous racism?
- Define the various underlying factors for vaccine hesitancy generally and for First Nations, Inuit and Métis peoples specifically
- Examine how colonialism, racism and mistrust challenge vaccine uptake amongst First Nations, Inuit and Métis populations, which directly impacts their health and health outcomes.
- Vaccine safety.
- Pregnancy and vaccination.
Leads
| Member | Postion |
|---|---|
| Selena Mills | Lead, Health Transformation & Strategic Communications: The Centre For Wise Practices in Indigenous Health, Women’s College Hospital |
| Lisa Richardson | Strategic Lead in Indigenous Health, the Centre For Wise Practices in Indigenous Health, Women’s College Hospital |
| Emily Simmonds | PhD. Candidate, Science and Technology Studies, York University |
| Ashley Migwans | Program Coordinator, Indigenous Health & Population Health and Social Medicine, University Health Network |
| Caroline Lindstone-Jones | Chief Executive Officer, Indigenous Primary Health Care Council |
| Nicole Blackman | Provincial Director, Indigenous Primary Health Care Council |
Planning, Research, and Knowledge Translation
| Member | Position |
|---|---|
| Rebecca Mador | Ontario Indigenous Culture Safety Team Lead, Indigenous Primary Health Care Council |
| Elisa Levi | RD, MPH, Independent Consultant |
| Kateri Gauthier | Indigenous Education Coordinator, the Centre For Wise Practices in Indigenous Health, Women’s College Hospital |
| Elder Diane Longboat | Aboriginal Services Elder, Shkaabe Makwa, the Centre for Addiction and Mental Health |
| Renee Linklater Shkaabe Makwa | Senior Director, Shkaabe Makwa, the Centre for Addiction and Mental Health |
| Harvey Manning | Director of Programs and Services Anishnawbe Health Toronto |
Language Translations
- Loretta Assinewai-Fox and Her Aunties
Graphic Design
| Member | Position |
|---|---|
| Bryn Ludlow | PhD. Candidate, Communications and Culture Studies, York University |
Video Production and Editing
| Member | Position |
|---|---|
| Lindsay Sarazin | Founder, Wolf Eye Productions |
| Emery Knight | Editor, Wolf Eye Productions |